Blood Pressure
Interconnected nature and potential of Lifestyle Health Pillars for preventing and reducing Hypertension.
by Hartmut Michael Günther, B.Sc. Hons. Biochemistry, Graduate Diploma Nutrition Medicine, Graduate Diploma Psychology
Contents
Introduction: Blood Pressure regulation; When is blood pressure High; Risks of prolonged, unmanaged Hypertension.
Primary & Secondary Hypertension. Definition. List of contributors to Primary Hypertension. Bidirectional influences.
Interventions: Medications. Non-Pharmacological. Interconnected synergistic nature and potential of Lifestyle Health Practices for preventing & reducing Hypertension.
Helping raise health literacy for clients needing to prevent, measure, manage or reduce elevated Blood Pressure. Inviting Input & Ideas. Send email to Hartmut and these inputs will be incorporated into this report
Appendix. Additional detail around the above contents. Plus, a colleague who is a Master Medical Librarian at the Burnie Hospital in Tasmania, agreed to conduct a
Literature Review entitled: Non-pharmacological interventions for Hypertension. Here are some of the highlights.
One Page Summary
Blood pressure is intricately maintained by the body within an optimal range. It does this so that that the trillion or so cells in our organs and deepest furthest reaches of the body get the oxygen and nutrients they need. And blood under pressure drives the elimination of waste that builds up. We are still on a journey that will give us the full picture of how the body does this.
Additionally, we don’t fully understand yet why in some of us, blood pressure increases beyond the safe range required for optimal health. We call this Hypertension.
We do know that hypertension is complex, multifactorial, bidirectional, and that how it manifests and responds to interventions is unique for every person.
We know that medications have some ability to reduce blood pressure. That they’re designed to target the body’s mechanisms of normal blood pressure control involving heart workload, fluid retention, blood vessel relaxation, enzymes, and hormones. And we know medications have side effects, again unique for every individual.
Importantly, we know that lifestyle or non-pharmacological interventions can bring down blood pressure close to or within a healthy range in most people. When this is difficult, or hypertension reduction is stubborn or resistant, judicious medication prescription in combination with lifestyle interventions is often successful.
The good News. The most effective lifestyle interventions for hypertension are a nutrition rich diet, movement that raises heart rate and increases strength, prioritising sleep, addressing mental health issues as they arise, understanding stress and indeed, our own behaviours. Plus, the ability to access, understand, evaluate, and use health information. There are more but the evidence is strong that these work effectively, particularly when practiced together.
More Good News. These practices & understandings (a better word than interventions) confer overall health and joy to any human. When practiced in combination they exponentially reduce the risks of other common modern day chronic health issues like heart disease, kidney disease, insulin resistance and diabetes, overweight, need for multiple medications and many more.
Introduction
This report mainly focuses on our understanding and subsequent practice and recommendations for our response to elevated blood pressure, also known as hypertension. While low blood pressure can also be problematic and dangerous, it will not be addressed here. There is extra information and details in the Appendix. However, the main gist is covered in the first 10 pages or so. (Before the appendix). There are lots of pictures.
Regulation of Optimal Blood Pressure.
The body uses a complex network of mechanisms to regulate blood pressure, including the nervous system, hormonal system, and local factors within blood vessels. Knowing a little about these mechanisms help understand how and why interventions work – both lifestyle and Pharmacological. All these mechanisms are interconnected and work in harmony to maintain blood pressure within the normal range.
The miraculous human body employs the following systems…
Renin-Angiotensin-Aldosterone System (RAAS)
This system plays a critical role in maintaining blood pressure. When blood pressure decreases, the kidneys release an enzyme called renin. Renin converts angiotensinogen (a protein produced by the liver) into angiotensin I, which is then converted into angiotensin II by angiotensin-converting enzyme (ACE). Angiotensin II causes blood vessels to constrict and stimulates the release of aldosterone, a hormone that prompts the kidneys to retain sodium and water, which increases blood volume and, consequently, blood pressure.
Baroreceptor Reflex
Baroreceptors are nerve endings located in the walls of the heart and blood vessels that detect changes in pressure. When blood pressure falls, these receptors signal the brain (specifically, the medulla oblongata) to increase heart rate and constrict blood vessels. Conversely, if blood pressure rises, the baroreceptors signal the brain to slow the heart rate and dilate blood vessels.
Vasopressin (also called Antidiuretic Hormone or ADH)
This hormone is released from the pituitary gland in response to a decrease in blood volume or an increase in the concentration of certain solutes in the blood. ADH acts on the kidneys to reabsorb more water, increasing blood volume and thereby increasing blood pressure. It can also cause constriction of blood vessels.
Atrial Natriuretic Peptide (ANP)
ANP is a hormone produced by the heart when it detects high blood pressure. ANP promotes salt and water excretion by the kidneys, which decreases blood volume and lowers blood pressure.
Autonomic Nervous System
The sympathetic and parasympathetic branches of the autonomic nervous system (ANS) play vital roles in blood pressure regulation. The sympathetic nervous system (part of the "fight or flight" response) can increase blood pressure by increasing heart rate and constricting blood vessels. In contrast, the parasympathetic nervous system (part of the "rest and digest" response) can decrease blood pressure by slowing heart rate.
Endothelium Derived Factors:
The endothelium, or lining of the blood vessels, produces substances that can either relax or constrict the blood vessels. Nitric oxide (NO), for example, is an endothelium-derived relaxing factor that helps keep blood vessels dilate, thus lowering blood pressure.
These systems are interconnected and work in harmony to maintain blood pressure within the normal range. Blood pressure is the force exerted by circulating blood on the walls of blood vessels
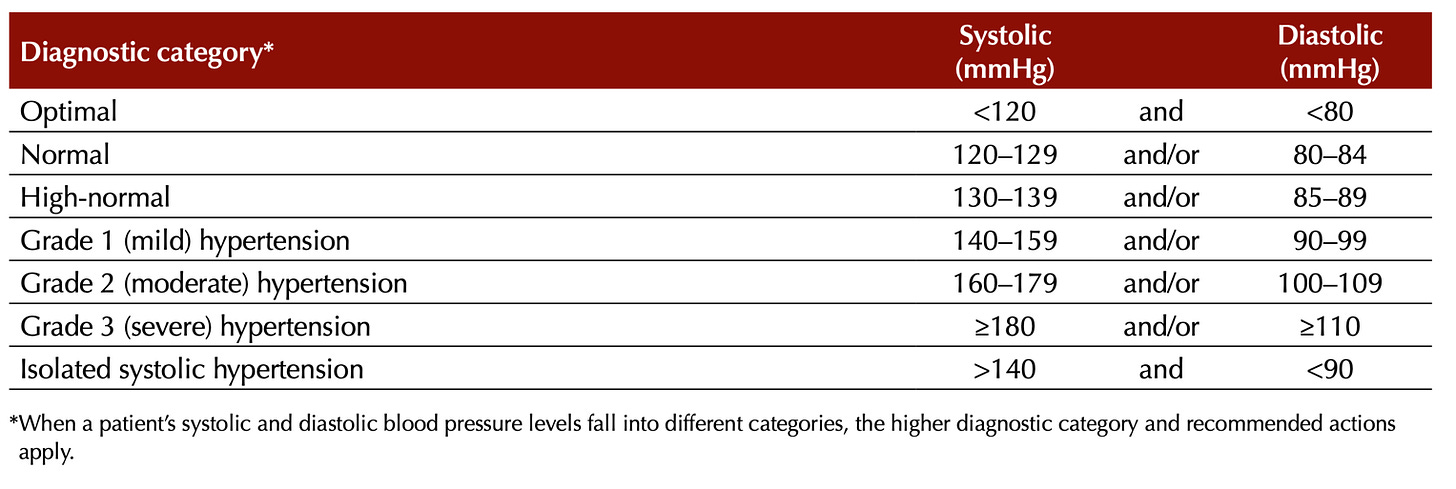
When is blood pressure high
Definition of Hypertension
Hypertension, commonly known as high blood pressure, is a medical condition characterised by persistently elevated blood pressure levels. Blood pressure is the force exerted by the blood against the walls of the arteries as the heart pumps it throughout the body. Hypertension occurs when this pressure consistentlyexceeds the normal range.
Next, we put into context what normal blood pressure means.
There are slightly different international and country specific guidelines and cut-off points that define when blood pressure is normal, high normal or classed as hypertension.
Australian and European understandings, wordings and guidelines are similar while the American cut off points that define hypertension are lower. There is controversy around this lower (US based) guideline.
Australian Clinic-based Classification of blood pressure levels in adults
From – Guideline for the diagnosis and management of hypertension in adults – 2016 – Heart Foundation
Also see more interesting data on these differences and how these contribute to people potentially being over diagnosed and indeed over medicated (based on the American cut-offs) - Blood Pressure Down Under, but Down Under What?
International and American Guidelines
From – The International Society of Hypertension
European Classification of Clinic blood pressure levels in adults
From - The Evolution of Hypertension Guidelines Over the Last 20+ Years: A Comprehensive Review
Risks of Prolonged Hypertension
This list, as shocking and unbelievable as it looks, shows some potential health risks associated with prolonged, unmanaged or out of control, high blood pressure.
Heads Up
Diagnosis of hypertension does not mean it will lead to all or any of the health issues listed below. However, if hypertension remains uncontrolled or increases over time beyond 140/80, so does the risk of developing some of these health issues. Nevertheless, every person is unique. Many factors like genetics, socioeconomic, nutrition, medication, self-knowledge, other lifestyle factors and the presence of other medical conditions, play their part. The risks that play out most commonly are shown first. The first 6 items alone should be enough to take hypertension seriously.
1. Cardiovascular disease: heart attacks, strokes.
2. Kidney damage: chronic kidney disease.
3. Vision problems: hypertensive retinopathy, blindness.
4. Aneurysm: risk of rupture.
5. Metabolic syndrome: obesity, diabetes risk.
6. Cognitive decline: dementia, Alzheimer's.
7. Pregnancy complications: preterm birth, low birth weight.
8. Sexual dysfunction: erectile dysfunction, reduced desire.
9. Sleep apnoea: disrupted breathing during sleep.
10. Arrhythmia: irregular heartbeats.
11. Enlarged heart: reduced pumping efficiency.
12. Increased risk of blood clots.
13. Weakened blood vessels: prone to rupture.
14. Reduced bone density: risk of osteoporosis.
15. Compromised immune system: infections, delayed healing.
16. Mental health concerns: anxiety, depression.
17. Impaired exercise capacity: reduced endurance.
18. Impaired wound healing: delayed recovery.
19. Organ damage: brain, heart, kidneys, eyes.
20. Risk of blood vessel rupture.
21. Increased risk of diabetes complications.
22. Impaired hearing: risk of hearing loss.
23. Mental health disorders: anxiety, depression.
24. Erectile dysfunction: male impotence.
25. Increased risk of complications during surgery.
26. Digestive issues: reflux, ulcers.
27. Increased risk of falls: balance, coordination.
28. Impaired liver function: liver disease.
29. Reduced fertility: men and women.
30. Increased risk of gallstones.
31. Complications in diabetes management.
32. Impaired respiratory function: shortness of breath.
33. Increased risk of gout: joint pain.
34. Increased risk of metabolic disorders.
35. Skin problems: spider veins, delayed healing.
36. Negative impact on bone marrow.
37. Increased risk of autoimmune disorders.
38. Adverse effects on mental well-being.
39. Increased risk of peripheral arterial disease.
40. Impaired lung function: pulmonary hypertension.
41. Complications during dialysis.
42. Increased risk of inflammation.
43. Adverse effects on bone health.
44. Impact on mental processing speed.
45. Complications during anaesthesia.
46. Increased risk of blood vessel inflammation.
47. Impact on gut health.
48. Altered brain structure.
Any Movement, particularly if we are mostly sedentary, at work or home, helps reduce risks associated with Hypertension
Primary & Secondary Hypertension
Contributors to Hypertension
Hypertension, or high blood pressure, is generally classified into two types: primary and secondary hypertension.
Secondary Hypertension
This type of hypertension is caused by an underlying health condition or certain medications. It usually appears suddenly.
Various conditions and medications can lead to secondary hypertension, including but not limited to - Kidney problems and some medications such as birth control pills, cold remedies, decongestants, over-the-counter pain relievers and Illegal drugs such as cocaine and amphetamines
Secondary hypertension is often resolved if the underlying condition is treated, or the triggering medication is stopped.
Primary (also called Essential) Hypertension
This is the most common type of hypertension, accounting for about 90-95% of all cases. The exact cause is not known. It is driven by a combination of factors listed next.
1. Genetic factors: Genetic variations can affect the renin-angiotensin-aldosterone system (RAAS), endothelial function, and sympathetic nervous system activation, leading to increased blood pressure.
2. Age: Aging can cause reduced arterial elasticity, increased arterial stiffness, and decreased responsiveness of the baroreceptor reflex, resulting in elevated blood pressure.
3. Ethnicity: Genetic factors and lifestyle factors in some ethnic groups can lead to increased sensitivity to salt, abnormal RAAS function, and other metabolic abnormalities, contributing to hypertension.
4. Obesity: Obesity can cause an increase in blood volume, activation of the RAAS, increased production of adipokines (hormones produced by fat cells), and inflammation, all of which can contribute to elevated blood pressure.
5. Diabetes: Diabetes can cause damage to blood vessels and kidneys due to high blood sugar levels and increased production of advanced glycation end products (AGEs), which can impair vasodilation and increase blood pressure.
6. Sedentary lifestyle: Physical inactivity can result in weight gain, decreased heart efficiency, and reduced nitric oxide production, leading to increased blood pressure.
7. Poor diet: High sodium intake can cause fluid retention and increased blood volume, while low potassium intake can reduce the ability to excrete sodium. Excessive alcohol consumption can lead to increased sympathetic nervous system activity and altered vascular function. High sugar, highly processed & takeaway foods and for some people, saturated fat intake.
8. Stress: Chronic stress activates the sympathetic nervous system and increases the production of stress hormones like cortisol, leading to vasoconstriction, increased heart rate, and elevated blood pressure.
9. Smoking and excess Alcohol: Chemicals in tobacco can cause inflammation, oxidative stress, and damage to blood vessel walls, leading to narrowing of blood vessels and increased blood pressure.
10. Sleep apnoea: Sleep-disordered breathing can cause intermittent hypoxia (low oxygen levels), which triggers the sympathetic nervous system, increases oxidative stress, and impairs endothelial function, raising blood pressure.
11. Kidney disease: Impaired kidney function can cause increased sodium and fluid retention, leading to increased blood volume and activation of the RAAS, which raises blood pressure.
12. Hormonal imbalances: Conditions like hyperthyroidism, hypothyroidism, Cushing's syndrome, and adrenal gland disorders can disrupt blood pressure regulation through various mechanisms, including altered RAAS function, increased cardiac output, and impaired vasodilation.
13. Medications: Some medications can cause fluid retention, increased heart rate, or vasoconstriction, leading to increased blood pressure. Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), oral contraceptives, and decongestants, can cause increased blood pressure.
14. Insulin Resistance and Metabolic Syndrome: Insulin resistance can lead to higher levels of insulin in the blood and although the relationship between insulin resistance and high blood pressure is complex and not yet fully understood, proposed mechanisms exist. See Appendix for more details.
The Good News. At least six of these factors contributing to Hypertension can be minimised through simple focused lifestyle modifications like Diet and Movement. Many of the others can be managed through medications.
Blood Pressure Interventions:
Medications
Hypertension can be managed by lifestyle factors like Diet, Healthy Weight, Sufficient Sleep, regular Movement, Stress awareness & more. Additionally, various categories of Medications are available that target different mechanisms of blood pressure control (mentioned earlier) in the body. Both lifestyle and medication interventions can be employed at the same time.
Sometimes hypertension medication treatment involves a combination of medications to effectively control blood pressure – especially in cases when high blood pressure is resistant to reducing to healthy levels. The downside of any medication is that there can be varying degrees of side effects. See Drugs.com for all side effects of any medication. For more on this see our previous post below -
Health Literacy and PolyPharmacy
In the previous post on Health Literacy we introduced in detail what is Health Literacy (HL), how it benefits us and then used a detailed example to show how it helps us if we have a chronic health condition. We used OsteoArthritis (OA) as an example. In breaking down the components of Health Literacy, we indicated that prevention is perhaps the first a…
Below is a list of major categories of medications used to treat hypertension, how they do it and some common brand names. Note that Medications are continually changing.
Diuretics: They work by helping the kidneys remove excess water and salt from your body, which reduces the volume of blood your heart must pump. | Thiazide diuretics: hydrochlorothiazide (Microzide), chlorthalidone | Loop diuretics: furosemide (Lasix), bumetanide (Bumex) | Potassium-sparing diuretics: spironolactone (Aldactone), eplerenone (Inspra)
Beta blockers: These reduce the heart rate, the heart's workload and the heart's output of blood, thereby lowering blood pressure. Examples: atenolol (Tenormin), metoprolol (Lopressor, Toprol-XL), propranolol (Inderal)
ACE inhibitors (Angiotensin-Converting Enzyme inhibitors): These block the formation of a natural body chemical called angiotensin II, which normally causes blood vessels to narrow. Examples: lisinopril (Prinivil, Zestril), benazepril (Lotensin), ramipril (Altace)
ARBs (Angiotensin II receptor blockers): Like ACE inhibitors, they block the action of angiotensin II, but instead of blocking its formation, they block its effect on your arteries. Examples: losartan (Cozaar), valsartan (Diovan), candesartan (Atacand)
Calcium channel blockers: They prevent calcium from entering the smooth muscle cells of the heart and arteries. When calcium enters these cells, it causes a stronger and harder contraction. Examples: amlodipine (Norvasc), diltiazem (Cardizem, Tiazac), verapamil (Calan, Verelan)
Alpha blockers: These reduce nerve impulses to blood vessels, which allows blood to pass more easily, causing the blood pressure to go down. Examples: doxazosin (Cardura), prazosin (Minipress)
Alpha-2 Receptor Agonists: These decrease the activity of the sympathetic (adrenaline-producing) portion of the involuntary nervous system. Example: clonidine (Catapres)
Combined alpha and beta-blockers: These are used in IV for hypertensive crises and are used in patients with a rapid heart rate. Example: labetalol (Trandate)
Central agonists: These prevent the brain from sending signals to the nervous system to speed up the heart rate and narrow the blood vessels. Example: methyldopa (Aldomet)
Vasodilators: These directly relax the muscles in blood vessel walls, causing the blood vessels to widen (dilate). Examples: hydralazine (Apresoline), minoxidil (Loniten)
Renin inhibitors: This is a newer class of drugs that works by decreasing certain chemicals that tighten the blood vessels, so blood flows more smoothly and the heart can pump blood more efficiently. Example: aliskiren (Tekturna)
Peripheral adrenergic inhibitors: These work by blocking neurotransmitters in the brain, which stops nerve signals to the blood vessels. As a result, the blood vessels become relaxed and less constricted. Examples: guanadrel (Hylorel), guanethidine mono sulfate (Ismelin)
Blood vessel dilators (vasodilators): Vasodilators are medications that open (dilate) blood vessels. They work directly on the muscles in the walls of your arteries, preventing these muscles from tightening and your arteries from narrowing. Examples: hydralazine (Apresoline), minoxidil (Loniten)
Aldosterone antagonists: These drugs block the effect of aldosterone, which is a hormone that can cause blood volume and blood pressure to rise. Examples: eplerenone (Inspra), spironolactone (Aldactone)
Blood Pressure Interventions:
Lifestyle factors for preventing, managing, and reducing Hypertension
There are LOTS! Here are the top ten. Based on general clinical guidelines and research here are the recommended most effective interventions for reducing hypertension (non-pharmacological), listed roughly in order of typical effect size.
Spoiler alert. While the effectiveness of interventions for reducing hypertension can vary based on individual factors like genetics, age, lifestyle, and overall health, adopting a healthy diet and exercise regimen, are usually considered the most impactful first-line interventions.
Additionally, the following interventions are often most effective when used in combination. There are many more like optimal sleep and mental health that for some people can be equally as effective at bringing down day to day blood pressure. See Appendix for more
1. Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and low in sodium can have a significant impact on blood pressure. The DASH (Dietary Approaches to Stop Hypertension) diet, for instance, has been shown to reduce blood pressure significantly. The DASH diet is based on the Mediterranean Diet with the addition of daily salt reduction. Healthy eating in general, particularly the Mediterranean style of eating, can help prevent or minimise hypertension, especially when combined with physical activity. See our series on the Mediterranean style of eating here -
Nuts and Seeds contribution to the Australian Mediterranean Diet
So much to say about the unpretentious nut. So many varieties originating from diverse areas of the globe. Such manifold array of nutrients and flavours spread throughout all the different nuts. So much health to be gained by bringing them into our eating regime.
2. Regular Physical Activity: Regular aerobic exercise, such as walking, jogging, cycling, or swimming, can lower blood pressure. The Australian Government Department of Health provides the following physical activity recommendations for adults aged 18-64 years, as outlined in the "Australia's Physical Activity and Sedentary Behaviour Guidelines" - Be Active Every Day: Engage in some form of physical activity every day. Accumulate 150 to 300 minutes of Moderate Intensity Physical Activity or 75 to 150 minutes of Vigorous Intensity Physical Activity, or an equivalent combination of both moderate and vigorous activities, each week.
Muscle Strengthening Activities: Include muscle strengthening activities on at least two days each week. This could include resistance training or exercises that use body weight for resistance (like yoga or Pilates). Minimize Sedentary Behaviour: Break up long periods of sitting as often as possible. Do More: More physical activity (up to several hours per day) and greater intensity activities provide additional health benefits. These guidelines are suitable for most adults irrespective of cultural background, gender or ability. One can also consider and incorporate high-Intensity Interval Training (HIIT) based on your physical abilities and guidance from a health professional.
3. Weight Management: Being overweight or obese increases the risk of hypertension. Losing even a small amount of weight can significantly lower high blood pressure. Slow and sustained or fast (2 weeks loosing 5kg) are options.
4. Limiting Alcohol and Avoiding Tobacco: Drinking alcohol in moderation (or not at all) and avoiding tobacco can lower blood pressure and overall cardiovascular risk. Smoking can cause a temporary spike in blood pressure and is a significant risk factor for heart disease. Note, that excessive drinking can raise blood pressure and reduce the effectiveness of blood pressure medications.
5. Reducing Sodium Intake: Consuming too much sodium can increase blood pressure. It's recommended to limit sodium intake to less than 2,300 milligrams (mg) a day, or even less (1,500 mg) for those with high blood pressure. Some people are more sensitive to the blood pressure increasing effect of salt than others. Find out where YOU fit in. Of course excess sweating (due to heat or sauna for instance) will increase need for salt and other electrolytes. Additionally eating potassium rich foods can also help.
6. Reduce Caffeine Consumption: While the link between caffeine and blood pressure isn't completely understood, it's still wise to limit caffeine intake, especially if you're sensitive to its effects.
7. Identify sources of Stress: What causes stress is UNIQUE for every person. Once you know the triggers you can more effetely manage it and recover (reduced blood pressure) more quickly. Monitor your self with a blood pressure measuring device till you know your triggers. For example - go for a 20 min brisk walk after a stressful and intense ZOOM meeting. Chronic stress can contribute to hypertension. Techniques such as deep breathing, yoga, and other relaxation techniques like walking in nature can help manage stress levels and reduce blood pressure. Chronic Stress and one’s Mental Health are in a bidirectional relationship. If you have a mental health condition like depression or anxiety, managing it effectively with the help of mental health professionals can also help control blood pressure. Ask for help.
8. Self-knowledge: or self-awareness, can play a significant role in managing hypertension, primarily through promoting healthier behaviours and lifestyle changes. Awareness of one's body and its reactions to certain foods, the impact of exercise, the need for rest can help in creating and sustaining healthier habits. Recognizing stress triggers and the part we play in bringing them into our lives. Self-knowledge can help in understanding what situations, thoughts, and emotions trigger stress. As stress can elevate blood pressure, managing it is crucial in controlling hypertension. Most importunately, understanding our own inner recourses and strengths is part of self-knowledge and contributes to developing self-efficacy, acceptance, and peace.
When you're relaxed, your body activates the parasympathetic nervous system which slows the heart rate, decreases blood pressure, increases intestinal and gland activity, and relaxes sphincter muscles in the gastrointestinal tract. Meditation can activate the parasympathetic nervous system, promoting a state of relaxation and helping to lower blood pressure. Off course meditation has the remarkable potential and ability to infuse us with boundless joy. See -
Meditation by any other name...
Sleep provides deep rest, peace and an opportunity to completely let go. Meditation provides deep rest, peace and an opportunity to completely let go, while we are awake.
9. Health literacy: refers to a person's ability to access, understand, evaluate, and use health information to make informed decisions about their health and healthcare. Health literacy plays a vital role in managing hypertension. Here's how:
Being better informed about one’s health. No one knows more about your body than you do. Articulating yourself empowers you in conversations with health professionals. People with high health literacy can more effectively communicate with healthcare providers. They can ask informed questions and better understand explanations, which can lead to more effective care.
Understanding Hypertension: High health literacy helps people understand what hypertension is, why it's a problem, and how it can be managed. They can learn about the risks associated with hypertension, such as heart disease and stroke, and how lifestyle modifications and medications can help control blood pressure. Navigating the Healthcare System: People with high health literacy can more effectively navigate the healthcare system. They can make appointments, understand their health insurance, and know when and where to seek help. Managing Medication: Health literacy is vital for understanding medication instructions, including when and how much to take, possible side effects, and potential interactions with other drugs. Other medications which are known to increase hypertension include non- steroidal anti-inflammatory drugs, steroids, angiogenesis inhibitors, tyrosine kinase inhibitors, atypical antipsychotics, antidepressants, amphetamines, hormone replacement therapy, immunosuppressants, and decongestants.
Lifestyle Modifications: People with high health literacy understand the importance of lifestyle modifications in managing hypertension. They can make informed decisions about diet, exercise, smoking, and alcohol consumption.
Self-Monitoring: Those with good health literacy are more likely to effectively self-monitor their blood pressure at home. They can understand what the numbers mean and when changes might indicate a need to consult with a healthcare provider.
10. Maintain Regular Check-ups: Regular medical check-ups ensure that your hypertension is being effectively managed and that any adjustments to your treatment can be made promptly. This also enables early detection and management of potential complications. Don’t be concerned in asking for help. If lifestyle changes aren't enough, medication may be necessary.
Appendix
Greater detail for many of the topics presented above…
Why have the blood under pressure. Regulation of Blood Pressure
The body uses a complex network of mechanisms to regulate blood pressure, including the nervous system, hormonal system, and local factors within blood vessels.
Adequate blood flow: Regulating blood pressure is essential for maintaining an adequate blood flow to all organs and tissues. This ensures that they receive a sufficient supply of oxygen and nutrients to function properly and effectively remove waste products.
Perfusion pressure: Blood pressure is critical for maintaining the perfusion pressure needed to drive blood through the microcirculation (capillaries). A sufficient perfusion pressure ensures that oxygen and nutrients are exchanged between blood and tissues, and waste products are removed.
Prevention of tissue damage: Excessively high blood pressure (hypertension) can damage the blood vessels and organs, particularly the heart, kidneys, brain, and eyes. Regulating blood pressure helps prevent such damage and reduces the risk of associated health issues, such as heart disease, stroke, and kidney failure.
Preventing circulatory collapse: Conversely, excessively low blood pressure (hypotension) can cause insufficient blood flow to vital organs, leading to inadequate oxygen and nutrient delivery. This may result in dizziness, fainting, and, in severe cases, circulatory collapse and shock.
Auto-regulation: Blood pressure regulation is necessary for maintaining the auto-regulation of blood flow in certain organs, such as the brain and kidneys. Autoregulation enables these organs to maintain a constant blood flow despite changes in blood pressure, ensuring their proper functioning.
Blood pressure is the force exerted by circulating blood on the walls of blood vessels
The relationship between blood flow and blood pressure
Blood flow and blood pressure are closely related physiological parameters that influence each other. Blood flow refers to the volume of blood being transported through the circulatory system per unit of time, while blood pressure is the force exerted by circulating blood on the walls of blood vessels. The following factors work together to maintain adequate blood flow and ensure that the body's organs and tissues receive the oxygen and nutrients they need.
Ohm's Law for Fluid Dynamics: Blood flow (Q) is directly proportional to the pressure difference (∆P) between two points in the circulatory system and inversely proportional to the resistance (R) offered by the blood vessels. Mathematically, it is represented as Q = ∆P / R. In this equation, an increase in blood pressure will result in an increase in blood flow if the resistance remains constant.
Resistance: Blood vessels, particularly arterioles, (blood vessel links between the arteries and the capillaries) can constrict or dilate to control blood flow to different organs and tissues. Vasoconstriction (narrowing of the blood vessel) increases the resistance, which in turn increases blood pressure and reduces blood flow. Conversely, vasodilation decreases resistance, leading to a decrease in blood pressure and an increase in blood flow.
Cardiac Output: Cardiac output is the product of heart rate (HR) and stroke volume (SV), which represents the volume of blood pumped by the heart per minute. An increase in cardiac output leads to an increase in blood pressure, which in turn can affect blood flow.
Blood Volume: The total volume of blood in the circulatory system also influences blood pressure. An increase in blood volume leads to an increase in blood pressure, while a decrease in blood volume can lower blood pressure. This relationship can affect blood flow as well.
Defining high blood pressure treatments and target cut-offs across countries and Age/Chronic conditions
From - Blood pressure: at what level is treatment worthwhile?
Insulin Resistance (IR) as a contributor to Hypertension
Insulin resistance is another factor that can contribute to high blood pressure. Insulin resistance occurs when the body's cells do not respond effectively to the hormone insulin, which regulates blood sugar levels. This resistance can lead to higher levels of insulin in the blood. The relationship between insulin resistance and high blood pressure is complex and not yet fully understood, but some of the proposed mechanisms include:
Increased sodium retention: Insulin resistance can cause the kidneys to retain more sodium, leading to fluid retention and increased blood volume, which raises blood pressure.
Activation of the sympathetic nervous system: Elevated insulin levels can activate the sympathetic nervous system, causing vasoconstriction (narrowing of blood vessels) and increased heart rate, both of which can raise blood pressure.
Endothelial dysfunction: Insulin resistance can impair the function of the endothelium, the inner lining of blood vessels. Endothelial dysfunction can reduce the production of nitric oxide, a molecule that helps to dilate blood vessels and maintain normal blood pressure.
Altered vascular smooth muscle function: Insulin resistance can alter the function of vascular smooth muscle cells, leading to increased arterial stiffness and high blood pressure.
Increased production of growth factors and inflammatory markers: Insulin resistance is associated with increased production of growth factors and inflammatory markers, which can contribute to blood vessel constriction and elevated blood pressure.
Evidence that High sodium intake can cause hypertension while low potassium intake can increase blood pressure
High sodium intake and low potassium intake have both been associated with hypertension. Here is a summary of the evidence supporting this relationship while keeping in mind that Individual responses to sodium and potassium intake may vary due to factors such as genetics, age, and underlying health conditions.
-------------------------------------------
Evidence that High Sodium intake and Low Potassium intake contribute to hypertension
High sodium intake:
Epidemiological studies: Observational studies have found that populations with higher sodium intake generally have higher blood pressure levels and an increased prevalence of hypertension. For example, the INTERSALT study, conducted across 32 countries, showed a strong correlation between sodium intake and blood pressure levels.
Clinical trials: Randomised controlled trials, such as the DASH-Sodium trial, have shown that reducing sodium intake can lead to a decrease in blood pressure. In this study, participants who followed a reduced sodium diet experienced a significant reduction in blood pressure compared to those on a higher sodium diet.
Meta-analyses: A meta-analysis of 34 randomized controlled trials found that reducing sodium intake led to a decrease in both systolic and diastolic blood pressure, especially in those with hypertension.
Low potassium intake:
Epidemiological studies: Observational studies have found an inverse relationship between potassium intake and blood pressure, meaning that lower potassium intake is associated with higher blood pressure levels. The NHANES study, for example, found that higher potassium intake was associated with lower blood pressure in the general population.
Clinical trials: Randomised controlled trials have shown that increasing potassium intake can lead to a decrease in blood pressure. For example, the DASH diet, which is rich in potassium, has been proven to reduce blood pressure in individuals with and without hypertension.
Meta-analyses: A meta-analysis of 33 randomised controlled trials found that potassium supplementation led to a decrease in both systolic and diastolic blood pressure, particularly in those with hypertension.
Additional Interventions:
Interconnected Synergistic Lifestyle factors for preventing, managing, and reducing Hypertension
1. Adequate Sleep: Chronic lack of sleep or poor-quality sleep has been linked to an increase in blood pressure. Ensuring you get a good night's sleep regularly can help in managing blood pressure.
2. Healthy Social Relationships: Positive social interactions and strong support networks can help manage stress levels and contribute to overall well-being, which can positively impact blood pressure.
3. Decreased Sugar Intake: Consuming a diet high in added sugars, particularly from sugary beverages, has been linked to high blood pressure. Reducing intake of these foods can help manage blood pressure.
4. Limit Processed Foods: Processed foods can be high in sodium and low in fiber and nutrients, contributing to increased blood pressure.
5. Regular Monitoring of Blood Pressure at Home: This can help you keep track of your progress, understand what may cause changes in your blood pressure, and alert you to dangerous levels that need immediate medical attention.
6. Potassium-Rich Foods: Increasing the intake of potassium-rich foods can help to balance out the negative effects of sodium and help to relax the blood vessels. Bananas, oranges, sweet potatoes, and spinach are all high in potassium.
7. Calcium and Magnesium in Diet: Adequate intake of these minerals has been linked to lower blood pressure. Dairy products, leafy greens, whole grains, poultry, and seafood are good sources.
8. Omega-3 Fatty Acids: Foods rich in Omega-3 fatty acids like fatty fish, walnuts, flaxseeds, and chia seeds can help lower blood pressure.
9. Avoid Long Periods of Inactivity: Sitting for long periods can lead to higher blood pressure. Try to incorporate movement into your day, even if it's just standing up or stretching every hour.
10. Limit Intake of Saturated and NO Trans Fats: These types of fats, found in many processed and fast foods, can raise blood pressure by contributing to the build-up of plaque in the arteries.
11. Regular Medical Check-ups: This allows for the early detection and management of high blood pressure and its complications.
12. Medication Adherence: For individuals who have been prescribed medication for hypertension, it's critical to take the medication as directed by the healthcare provider. This helps to maintain the effectiveness of the treatment.
13. Limit Canned or Packaged Food: Such foods often contain high levels of sodium and preservatives, which could contribute to increased blood pressure.
14. Proper Management of Other Chronic Conditions: If you have conditions like diabetes or high cholesterol, managing them effectively can also help control your blood pressure.
15. Limit Red Meat: Red meat is often high in saturated fats and has been linked with higher blood pressure in some studies. Opting for lean proteins like chicken, fish, or plant-based proteins can be a healthier choice.
16. Mindful Eating: Being aware of what and when you're eating can help prevent overeating and promote a balanced diet.
17. Avoid Heavy Metal Exposure: Chronic exposure to heavy metals such as lead can lead to increased blood pressure.
18. Avoid Noise Pollution: Chronic exposure to noise pollution has been associated with increased stress levels and hypertension.
19. Environmental Temperature: Both extremely cold and hot temperatures can put stress on the heart, leading to increased blood pressure. Try to stay in a moderate, comfortable environment as much as possible.
20. Maintaining Good Dental Hygiene: Some research suggests that periodontal disease (gum disease) might be associated with high blood pressure.
21. Breathing Exercises: Certain breathing techniques, like slow, deep breathing exercises, can help relax your body and lower your blood pressure.
22. Biofeedback and Neurofeedback: These techniques can teach you how to consciously control bodily functions that normally occur involuntarily, such as heart rate, which could help in managing blood pressure.
23. Probiotic & Prebiotic foods: Emerging research suggests that maintaining a healthy gut microbiota by using probiotics could be beneficial in managing hypertension, although more research is needed in this area.
24. Avoidance of Endocrine Disrupting Chemicals: Some chemicals found in everyday items such as plastic containers, cans, and cosmetics can interfere with the body's endocrine system and potentially increase blood pressure.
25. Good Posture: Maintaining good posture might help to improve circulation and oxygenation of your body, indirectly affecting blood pressure.
26. Healthy Workplace Environment: Working in a stressful or unhealthy work environment can increase your stress levels, indirectly contributing to high blood pressure.
27. Avoid High Altitude Environments: At high altitudes, the air is thinner and oxygen levels are lower, which can put more pressure on your heart and lungs to supply the body with oxygen, possibly increasing your blood pressure.
28. Limit Exposure to Light at Night: Some research suggests that exposure to light at night can interfere with your body's circadian rhythms, leading to increased stress and potentially higher blood pressure.
29. Wear Loose Clothing: Tight clothing can restrict blood flow, leading to increased blood pressure.
30. Music Therapy: Listening to calming music may help lower stress levels, and subsequently blood pressure.
31. Massage Therapy: Regular massages may help to reduce stress and tension, which can aid in managing blood pressure.
32. Heat Therapy: Activities like sauna use or hot baths can potentially help lower blood pressure by causing blood vessels to expand, though people with high blood pressure should be cautious with these activities.
33. Cold Therapy: Some advocate cold showers or other cold therapies to stimulate circulation and metabolism, though its direct effect on blood pressure is unclear.
34. Mindful Consumption of News and Social Media: Overexposure to news and social media can induce stress and anxiety, which can contribute to high blood pressure.
35. Pet Ownership: Some research has shown that owning pets, particularly dogs, may help lower blood pressure and reduce stress.
36. Spending Time in Nature: Activities like forest bathing (spending time in a forested area) can help to reduce stress levels and subsequently lower blood pressure.
37. Sexual Activity: Regular sexual activity, which can be a form of exercise and stress relief, might help in managing blood pressure.
38. Therapeutic Touch and Hugging: Physical contact, such as hugging, has been shown to help lower stress levels, which could indirectly help manage blood pressure.
39. Involvement in Meaningful Activities or Hobbies: Engaging in activities that you find enjoyable or meaningful can help to reduce stress and could potentially contribute to lower blood pressure.
40. Laughter and Humour: Some research suggests that laughter can help to lower stress hormones, reduce inflammation in the arteries, and increase "good" HDL cholesterol, all of which can help lower blood pressure.
41. Volunteering and Community Involvement: Engaging in altruistic behaviors such as volunteering can help reduce stress levels, which could indirectly help manage blood pressure.
42. Positive Affirmations and Visualization: These techniques can help reduce stress levels and promote a positive mindset, potentially impacting blood pressure management.
43. Structured Daily Routines: Maintaining regular sleep, eating, and activity routines can contribute to overall health and stress management, indirectly influencing blood pressure.
44. Sunlight Exposure: Moderate sunlight exposure can help the body produce vitamin D, which has been associated with lower blood pressure in some research.
45. Reduced Use of NSAIDs: Over-the-counter medicines like nonsteroidal anti-inflammatory drugs (NSAIDs) can potentially raise blood pressure. Limit their use under the advice of a healthcare provider.
46. Balanced Electrolytes: Electrolyte imbalances can potentially impact heart rhythm and blood pressure. Maintaining a balanced intake of electrolytes such as sodium, potassium, calcium, and magnesium is important.
47. Reducing Toxin Exposure: Chronic exposure to certain environmental toxins and pollutants could potentially contribute to hypertension.
48. Mindful Technology Use: Overuse of digital devices can potentially contribute to stress and sedentary behaviour, which might indirectly impact blood pressure.
49. Control of Allergies: Uncontrolled allergies can lead to inflammation and stress on the body, which can potentially impact blood pressure. Proper management of allergies can contribute to overall well-being and potentially aid in managing hypertension.
50. Reduced Screen Time: Spending excessive time in front of screens (TV, computer, smartphone) can contribute to a sedentary lifestyle and increased stress levels, which could indirectly affect blood pressure.
51. Managing Chronic Pain: Chronic pain can increase stress levels and have an indirect impact on blood pressure. Proper pain management can, therefore, potentially contribute to hypertension management.
52. Meditative Movement Practices: Practices such as tai chi, qigong, and yoga combine physical movement, meditation, and breathing exercises, which can help reduce stress and potentially aid in managing blood pressure.
53. Improving Indoor Air Quality: Exposure to indoor pollutants and allergens can contribute to cardiovascular health issues, potentially including hypertension.
54. Balancing Work-Life Activities: Ensuring a good balance between professional and personal activities can help manage stress levels, contributing to better blood pressure control.
From the research
A colleague who is a Master Medical Librarian at the Burnie Hospital in Tasmania, agreed to conduct a Literature Review entitled:
Non-pharmacological interventions for Hypertension.
Here are some of the highlights…
Effects of Comprehensive Lifestyle Modification on Blood Pressure Control - link
Conclusion: Individuals with above-optimal BP, including stage 1 hypertension, can make multiple lifestyle changes that lower BP and reduce their cardiovascular disease risk.
Critical review of nutrition, blood pressure and risk of hypertension through the lifecycle: do B vitamins play a role? - link
Peer Reviewed version is here
From Abstract: …emerging evidence has identified a novel role for one-carbon metabolism and the related B vitamins, particularly riboflavin, in BP. Specifically in adults genetically at risk of developing hypertension, owing to the common C677T polymorphism in MTHFR, supplemental riboflavin (co-factor for MTHFR) was shown in randomised trials to lower systolic BP by up to 13 mmHg. A BP response to intervention of this magnitude could have important clinical impacts, given that a reduction in systolic BP of 10 mmHg is estimated to decrease stroke risk by 40%.
Hypertension - Do Inflammation and Immunity Hold the Key to Solving this Epidemic? - link
Very Interesting albeit very detailed & complex …Investigating the immune system involvement in Hypertension.
Hypertension in older adults: Assessment, management, and challenges - link
“Hypertension increases with age, with its prevalence increasing from 27% in patients aged younger than 60 years to 74% in those aged older than 80 years.4 The Framingham Heart Study5 showed than more than 90% of the participants with a normal blood pressure (BP) at age 55 years eventually develop HTN. Approximately 60% of the population has HTN by 60 years of age and about 65% of men and 75% of women develop high BP by 70 years.”
The Gut Microbiome in Hypertension
Recent Advances and Future Perspectives. “The intricacies of the role of the microbiome in hypertensive disease is a matter of ongoing research, and there are several technical considerations which should be accounted for moving forward. In this review we provide insights into the host-microbiome interaction and summarize the evidence of its importance in the regulation of blood pressure." - link
Effect of a Walnut Diet on Office and 24-Hour Ambulatory Blood Pressure in Elderly Individuals
“Among nuts, walnuts are particularly well suited to have BP effects because they contain little sodium and possess a complex nutrient matrix, including sizable amounts of bioactive molecules: ALA, the vegetable n-3 fatty acid, the metabolism of which gives rise to vasodilatory and anti-inflammatory oxylipins; γ-tocopherol, a form of vitamin E active in reducing oxidation and inflammation; non-sodium minerals with BP-lowering effects such as potassium, magnesium and calcium; arginine, the amino acid precursor of the endogenous vasodilator nitrous oxide; and characteristic polyphenols disclosing potent anti-oxidative and anti-inflammatory actions. Indeed, walnuts are the only nut type shown to consistently improve endothelial function in controlled trials testing nut diets for effects on vascular reactivity.” LINK
Impact of therapeutic lifestyle changes in resistant hypertension
This paper reviews key studies that quantify the blood pressure lowering effects of certain therapeutic lifestyles in patients with Resistant Hypertension. - LINK
Mechanistic Links Between Obesity, Diabetes, and Blood Pressure: Role of Perivascular Adipose Tissue - link
A very lengthy fascinating paper that highlights the links between obesity, diabetes and Blood Pressure and goes deep, deep down into the cellular metabolism of adipose tissue.